Separating fact from fiction using pharmacogenetics

The same drug can be given to two patients with the same diagnosis, in the same dosage and at the same time, and they can still respond differently. Understanding what drives these differences in response is a major component of the pharmaceutical sciences work we do at St. Jude Children’s Research Hospital. This type of science also underlies the Clinical Pharmacogenetics Implementation Consortium (CPIC) which is co-led by me and Dr. Teri Klein of Stanford University, and directed by Dr. Kelly Caudle of St. Jude.
Pharmacogenetics describes the influence genes have on drug effects among different patients. CPIC brings together leaders in pharmacogenetics to provide guidance on how to use genetic testing to guide clinical prescribing decisions. This can include which treatments to use, when to use them, how they should be dosed and how to combine them with other types of treatments.
The idea of using genes to tell us how to best use certain drugs has tremendous appeal. But in practice there are many considerations, and often hurdles, to surmount to appropriately use pharmacogenetics for clinical care. At the 2019 CPIC meeting, St. Jude played host to robust discussions among pharmacogenetic experts from around the country and internationally about the roadblocks and best practices surrounding this field.
Pharmacogenetics in an electronic age
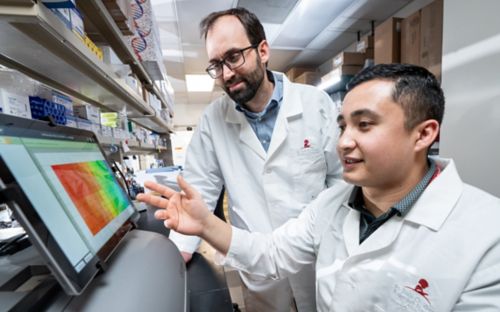
One of the most prominent topics at the CPIC annual meeting was how to standardize pharmacogenetic information for integration into electronic health records. Pharmacogenetics is most useful when clinicians have access to information during clinic visits. In many instances this means embedding pharmacogenetic information in a patient’s electronic health records or creating a clinical decision support tool that can integrate with electronic health record systems.
Electronic health records are not standardized across all healthcare providers. There are different vendors, whose products provide varying functionality. Additionally, hospitals and individual doctors often do things differently, for example using their own terminology. It may seem like a small thing, but standardizing terms is crucially important for integrating pharmacogenetics into electronic health record systems. Vendors who make these systems need standardized terms to create a product that will work for all of their customers, not just a single hospital.
To address some of the variation that hinders pharmacogenetic information from working in electronic health record systems, CPIC led a survey to help standardize pharmacogenetic terms. This initial work, which was published in 2017 has shown some progress toward standardization, but there is still much to do to unify the field. CPIC is now turning toward the more difficult genes, where there is less consensus to try to bring clarity to their use and standardize recommendations.
Myth-busting for non-actionable genes
Another project taken up by CPIC is the development of guidelines to help clinicians evaluate genes for which there is a lack of evidence supporting their use. Too many times, such genes are promoted by genetic testing companies claiming a clinical purpose. In reality, the evidence for such use does not exist or is not conclusive, meaning such genes shouldn’t be used to guide treatment decisions.
The gene MTHFR exemplifies this problem. As a group, CPIC has found that the gene-drug associations known for MTHFR don’t have the necessary evidence to be incorporated into clinical care. Yet, the internet is full of websites touting a link between MTHFR and dosing of the chemotherapy methotrexate, as well as risk of many diseases. Helping to get the word out about MTHFR, and other genes for which there are dubious claims of clinical utility in pharmacogenetics, is an important part of the work CPIC plans to undertake going forward.
CPIC has an opportunity to provide leadership and guidance in the at times murky field of gene-drug relationships. As genetic testing has become more widespread, it is increasingly important to have clear medically and scientifically vetted information about pharmacogenetics. Working together will help us provide much needed clarity to clinicians and patients, making the work of a cooperative group like CPIC more important than ever.