New model mimics progression of pediatric bone marrow failure

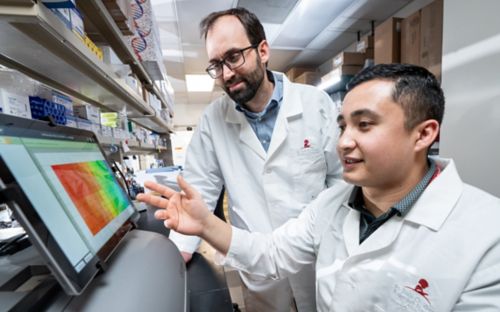
Co-first authors Melvin Thomas, PhD, and Sherif Abdelhamed, PhD, (L to R), led the creation of a new model of pediatric bone marrow failure.
Mysteries have captivated people for generations. From Sherlock Holmes to the cast of CSI, intrepid investigators need clues to solve a case. Until recently, researchers had too few clues to understand why children develop myelodysplastic syndromes (MDS) and related bone marrow failure disorders. MDS is a group of rare disorders in which bone marrow fails to make enough healthy blood cells. MDS is more common in adults but can develop in children. The pediatric version has different causes, which are not well understood.
In 2017, Jeffery Klco, MD, PhD, St. Jude Department of Pathology, helped discover a clue that unlocked MDS research. He found that germline mutations in the genes SAMD9 and SAMD9L were a new cause of genetic predisposition for MDS in some pediatric patients. Despite this advance, tantalizing mysteries remained. For example, children in the same family, with the same mutation, can have different outcomes – one can develop bone marrow failure while the other is unaffected. In some patients, a whole chromosome is lost.
Members of the Klco lab realized they needed more clues. Just like the iconic magnifying glass of a private investigator, the researchers’ progress required a tool to find out new clues about the disease.
Making a model of MDS
Klco and his colleagues recently reported on a new mouse model of germline SAMD9L mutations – the clue-finding tool the field needed. The work appeared in the Journal of Clinical Investigation. The researchers’ model has one of the disease-causing mutations previously described by the Klco lab in the mouse Samd9l gene. Over time, some of the mice with the mutation developed bone marrow failure, like what is observed in some patients with these mutations.
“The mouse strain we generated nicely recapitulates the phenotypes that we see in patients,” Klco said. “Not only does it give us a much better understanding of why kids with these mutations develop MDS and bone marrow failure, but it also gives us a good in vivo model system to do further discovery, test therapeutics and make additional advances.”
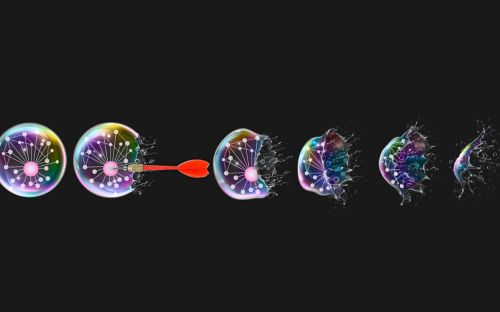
Duplicating the mystery of disappearing DNA
Each human has 46 DNA chromosomes – 23 from each parent. In MDS, patients lose the copy of chromosome 7 that has the mutated SAMD9 or SAMD9L gene. Losing a copy of a chromosome is potentially very detrimental. Chromosome loss can affect growth, development and body functions. Having only one copy of a chromosome is called monosomy.
As the scientists characterized the model, they were surprised by how faithfully it captured many aspects of the disease in humans, including some of the stranger characteristics of this syndrome. For example, mouse blood cells deleted the chromosome with the disease-causing mutation, mirroring the event observed in humans.
“Despite having germline mutations in either SAMD9 or SAMD9L, both of which are located on chromosome 7, the patients will commonly develop MDS with monosomy 7,” Klco said.
Monosomy 7 occurs when patients lose one of their two copies of chromosome 7. “The monosomy 7 clone always lacks the germline mutation in SAMD9 or SAMD9L, suggesting that the development of monosomy 7 is a compensatory response to cellular defects caused by the mutation.”
“I did not expect that to happen in mice” he continued. “Surprisingly, a few mice developed a deletion on mouse chromosome 6, the equivalent to losing human chromosome 7. It was the same phenomenon where the cells that were growing had deleted the disease-causing germline mutation. That was interesting to see.”
Inflammation is an issue for MDS
The researchers also found a major clue about why only some people with the causative mutations develop symptoms of MDS by studying inflammation. In the researchers’ mouse model, inflammation directly impacted disease development. Inflammation is the group of chemical signals released by damaged or infected tissues to tell the immune system ‘There is a problem here.’ However, inflammation itself can be damaging and cause problems. All the mice that developed a deletion in chromosome 6 (equivalent to chromosome 7 and the loss of SAMD9/SAMD9L in humans) were those challenged with inflammation.
“We're increasingly recognizing the importance of bone marrow inflammation in MDS and bone marrow failure,” Klco said. “The other intriguing thing is that these mutant genes are upregulated in response to inflammation. We can very easily imagine a model where inflammation causes increased expression of these genes, which ultimately collaborates with the mutation to drive the disease in patients.”
In addition to the chromosome deletion and inflammation, the model showed another clue – a defect in B-cell production. B cells are immune cells that produce antibodies to give long-term protection against disease. The investigators were initially surprised to see this – but during the same time they developed their model, new clinical data showed a B-cell deficit in human patients with germline SAMD9 or SAMD9L mutations. This provides further evidence that the model will be useful in the future to study the diverse impact of these mutations.
“It is fascinating how we were able to generate a mouse model that mimics the characteristics seen in patients with SAMD9L mutations,” said co-first author Sherif Abdelhamed, Ph.D, a senior scientist in Klco’s lab. “Now that we have this model, we can learn how mutant Samd9l leads to bone marrow failure and chromosomal deletion, and the role of the inflammatory microenvironment in this context. Our goal is to continue understanding the disease pathogenesis and hopefully contribute to controlling it.”
The scientists cannot predict what clues they will find with their new mouse model, but it brings the field of pediatric MDS and bone marrow failure one step closer to discovering more effective treatments for children with these diseases.