Genetics: The myth of the monolith: How molecular groups can improve cancer care

Molecular groups are clusters of patients whose cancers are driven by the same underlying biology. Scientists at St. Jude are studying molecular groups to better understand and treat many types of cancer.
The discovery of the double helix structure of DNA in 1953 was the culmination of many years of effort, yet it was also the starting point for a genetic age. That discovery launched scientists’ ability to tease information out of our genes and would transform our understanding of human health and disease. From the 1979 discovery of TP53, the most commonly mutated gene in cancer, there flowed a new understanding that cancer harbors different mutations. These genetic abnormalities not only make cancer different from healthy tissue but can distinguish between different types of cancer. The idea that cancer is a monolith, indivisible and uniform, was undeniably proven to be a myth by genetics. Cancers instead contain a complex set of different mutations, capabilities and vulnerabilities that require a diverse set of strategies to treat.
It is perhaps not surprising that cancers that occur in different tissues, such as the blood and the brain, are often very different in their genetic makeup and how they behave despite sharing some basic similarities, such as unchecked cell growth. But even cancers that arise from the same tissue, such as different types of blood cancer, can harbor a variety of genetic mutations and require different treatment approaches. There are tremendous implications for treatment by drilling down into the many different subtypes and molecular groups of cancer to understand its complex nature and vulnerabilities.
Targeted therapies that lock onto an aspect of the cancer’s biology, such as a specific genetic mutation, deliver therapy in a guided way. With the advent of these therapies, it has become increasingly important to understand the genetic underpinnings of cancer. Having a type of cancer for which targeted therapy is available can put a patient on a more effective treatment track. Additionally, understanding the mutations in a cancer can help physicians and patients understand the patient’s risk of relapse – which is important because there are things that physicians can do to help prevent recurrences in patients who are high risk, such as a longer duration of therapy.
Scientists at St. Jude are at the forefront of understanding the landscape of pediatric cancer, sifting through enormous amounts of data to stratify patients according to the subtype or molecular group that corresponds with the genetic abnormalities in their cancer. This work is shaping the design of future clinical trials and helping to improve cancer care today.
Charting the pediatric leukemia roadmap
Scientists at St. Jude recently created a roadmap of the genetic mutations present in the most common childhood cancer, acute lymphoblastic leukemia (ALL). The study was the first to supply a comprehensive view of the genomics of all subtypes of ALL. Led by Charles Mullighan, MD, St. Jude Comprehensive Cancer Center deputy director, and Jinghui Zhang, PhD, St. Jude Department of Computational Biology chair, the study serves as a foundational guide for physicians and scientists to understand disease development and improve treatment outcomes.
“Because of the scale of the study, we could identify many newly implicated genes that have not been reported in leukemia or cancer at all and show that they fall into several new cellular pathways,” Mullighan said.
The study, published in Nature Genetics, was unique because it included 2,574 pediatric ALL patient samples, the largest such cohort ever published. As a comparison, earlier studies have typically examined hundreds of samples or fewer. St. Jude investigators collaborated with the Children’s Oncology Group to collect samples over more than a decade.
The researchers found that, on average, the pediatric cancer samples had just four mutations that drove the development of ALL. They identified 376 significantly mutated genes that potentially drive cancer development, 70 of which have never been implicated in ALL. The researchers also found differences in the mutations present in subtypes of ALL, which may affect clinical care. For example, two of these groups involved specific genetic rearrangements that differed by CEBPA/FLT3 or NFATC4 gene expression. This observation may have clinical implications, as new FLT3 inhibitors are in clinical trials, suggesting the CEBPA/FLT3 ALL subtypes may be sensitive to such therapies, but the other subgroup may not be.
“The study demonstrates the power of the data,” Zhang said. “If you don't have a sufficient number of patient samples, you lack the statistical power to find drivers present at a low prevalence. Once we had the power, we found a subgroup of new drivers involved in ALL development.”
Understanding the hidden drivers of brain cancer
In addition to her work on leukemia, Zhang is also bringing the power of big data to childhood brain tumors. In Acta Neuropathologica, Zhang and Jason Chiang, MD, PhD, St. Jude Department of Pathology, revealed a novel cause of aggressive pediatric brain cancer. The study was the first to document how a transposon, a piece of DNA that “jumps” around the genome, can donate its promoter to drive the expression of an oncogene
Transposons are repetitive sequences of DNA that make up about 17% of the human genome and can move around. Long Interspersed Element-1 (LINE-1 or L1) is the only active transposon in humans. On average, the human genome contains approximately 80-100 active L1s. L1s are considered mostly benign, a genetic remnant that resembles a gene. Like most genes, L1s have segments of DNA that regulate their expression. A promoter is part of the cellular machinery responsible for regulating expression at certain sites in the genome. Zhang and Chiang found that retrotransposition, the “jumping” of L1, brought an active promoter to an oncogene, FOXR2. This led to overexpression of FOXR2 and, ultimately, cancer.
The work advanced the understanding of high-grade glioma, an aggressive brain cancer that is often resistant to treatment. This new understanding of biology can guide new avenues of research into these tumors.
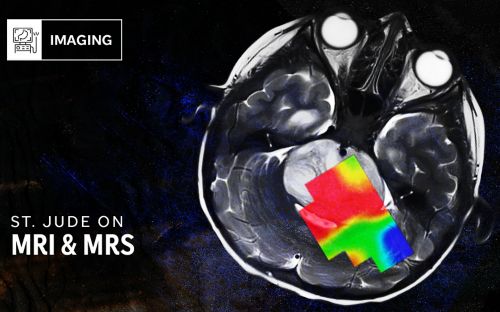
Landmark brain tumor papers highlight molecular groups
Understanding medulloblastoma, a common type of malignant childhood brain tumor, also relies on molecular profiling. Research by St. Jude scientists and others has classified medulloblastoma into four distinct molecular groups: WNT and SHH (which are driven by their namesake genetic mutations), Group 3 and Group 4. The prognosis for medulloblastoma is different for each molecular group. Retrospective analyses have shown that WNT tumors respond to treatment the best, with a 95% five-year survival rate. SHH and Group 4 tumors have approximately 75% five-year survival, and Group 3 has 60%.
Scientists at St. Jude published two papers covering the results of the SJMB03 clinical trial and a detailed look at relapsed medulloblastoma using data from SJMB03 and SJYC07 in the Journal of Clinical Oncology. In both the clinic and the lab, results underscore the need for integrated molecular assessment of these tumors. For example, the researchers identified new risk groups from SJMB03 within the previously established molecular groups. They found that all WNT, and some SHH and Group 3/4, are low risk. However, scientists also found that some SHH and Group 3/4 are high-risk.
“This study has given us a more granular understanding of risk that can help us determine when to reduce or escalate therapy,” said Giles Robinson, MD, St. Jude Department of Oncology.
Additionally, the study of relapsed medulloblastoma found that 10% of tumors classified as relapsed medulloblastoma are secondary malignancies. Most often, these secondary cancers, which are known to occur as a result of prior treatment, are high-grade gliomas. This is an essential distinction because newly diagnosed high-grade glioma and relapsed medulloblastoma may receive different treatments.
This study also found that while most tumors remain in the same molecular group from diagnosis to relapse, this is not always the case. The researchers found evidence of subgroup switching between Group 3 and Group 4 tumors. Conventional wisdom suggested that the genetic makeup of tumors can change dramatically from diagnosis to relapse, but this study also provides evidence that tumors are more genetically stable from diagnosis to relapse than previously thought.
“We’ve been able to provide important context to the patterns of relapse that we see in childhood medulloblastoma,” said corresponding author Paul Northcott, PhD, St. Jude Department of Developmental Neurobiology. “These findings underscore the need to include molecular analysis in the diagnosis and treatment of these tumors, both in the frontline and relapse settings.”
Many diseases under one banner
No matter what type of cancer researchers investigate, the information contained in our genes is of crucial value for understanding what drives cancer, how it might behave, what weaknesses might be exploited therapeutically, and how to tailor therapies. While the notion of cancer as a monolith with a single cure is a relic of the past, that history is also a testament to the power of the genetic innovations that have taken root in cancer research over the past 70 years. Every new discovery that helps distinguish one type of cancer from another pushes the field closer toward new and unique therapies that strive to improve treatment for every type of cancer.