TP53: One important gene in rare cancers - an update

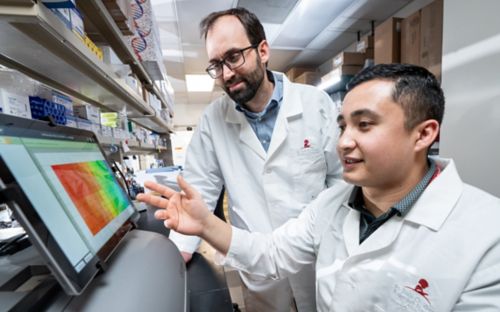
In this pre-COVID-19 photo from 2018, a St. Jude clinical and research team have found ways to identify and treat such rare diseases as ACT, Li-Fraumeni syndrome and Beckwith-Wiedemann syndrome. New research has found that a second variant in a tumor suppressor gene can greatly increase a person's risk of developing cancer.
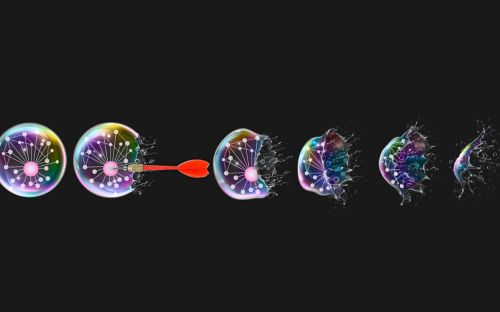
Cell division, the process of making new body cells, is a lifelong process. If you live to an average age, your body cells will divide about 10,000 trillion times. That’s one, followed by 16 zeros.
In any one of these divisions, just one mistake could be the beginnings of a tumor.
The TP53 gene: one of the most important genes in cancer research
I study the molecular biology of pediatric adrenocortical tumors, a rare disease. And because of the strong association with a genetic defect in the TP53 gene, I’m also interested in this gene.
The TP53 gene is responsible for monitoring cell division in your body. If a cell’s DNA is damaged or improperly copied, TP53 stops the cell from dividing. TP53 can correct the damage, prevent replication or send an apoptotic message, forcing the cell to die. In effect, the TP53 gene is the guardian of your genome.
We’re learning more about cancers and other conditions associated with TP53 mutations, including adrenocortical tumors (ACTs) and Li-Fraumeni syndrome. Our ACT research has also led to more information about Beckwith-Wiedemann syndrome.
“If a child has an adrenocortical tumor, many times, it’s because they have an inherited TP53 mutation,” says Gerard Zambetti, PhD, associate director of training and education for the St. Jude Comprehensive Cancer Center. “But there are other ways of getting to that same tumor type.”
But what about ACTs that are not showing germline mutations in the TP53 gene? This question left our team and the clinical team with a problem to solve. Our work published in the Journal of Clinical Oncology showed how some ACT cases can also occur through a germline, or inherited, defect in chromosome 11p, and some others because of an unidentified molecular event.
ACT and the Brazilian story
Years ago, Raul Ribeiro, MD, worked at St. Jude as a fellow. He then returned home to practice in Brazil and noticed a high incidence of ACT in children. He returned to St. Jude and began to organize the International Pediatric Adrenocortical Tumor Registry (IPACTR), collecting clinical and demographic data from pediatric patients with ACTs around the world.
Pediatric ACT is rare in the U.S., occurring in about 1 in 3 million children. In Brazil, pediatric ACT occurs 15 times more often. Dr. Ribeiro and his team showed that ACTs in Brazilian patients were all associated with the same inherited TP53 mutation, even though the children were from different families.
I determined that this single mutation, TP53-R337H, could be traced back several generations, and is the same for all Brazilian patients. Because the registry developed at St. Jude we have traced this mutation in patients from Portugal and Spain, it led us to the hypothesis that this mutation originated in Iberic Peninsula and spread to Brazil..
We learned that all of these families have the same founder mutation. Some families with the mutation have cancers of all kinds, like Li-Fraumeni syndrome, where catastrophic mutations in TP53 result in a nearly 100 percent chance of developing cancer, sometimes multiple cancers, and usually at a young age. But other Brazilian families have little or no instances of cancer. This suggests other environmental or genetic interactions with the mutations may be involved.
Through the International Pediatric Adrenocortical Tumor Registry, physicians around the world began sending medical and demographic information about their ACT patients. They also sent blood and tumor samples to give us more data for our research.
More screening and education needed
Because ACT can show up for quite different reasons, it’s important for patients and their families to find out the driver of that tumor.
A child with a TP53 mutation is at a higher risk for cancer. If a child is tested and found to have a mutation in this gene, then the child’s siblings and family members can also be checked for the mutation. That information is critical in terms of future screening and surveillance.
Through whole-genome sequencing and other projects, we are learning more about the genetic events that lead to benign and aggressive cases. We recently published in Science Advances the results of a whole-genome sequencing study focused on individuals of Brazilian ancestry who have the TP53-R337H founder mutation. We found that in some people, a second variant in the tumor suppressor gene XAF1 occurs. Together these inherited variations in TP53 and XAF1 can greatly increase a person’s risk of developing cancer.
Our research and clinical team remain committed to investigating unknown instigators of this disease and furthering treatment options. Indeed, our molecular analysis of adrenocortical tumors in the lab can inform clinical decisions regarding the effectiveness of specific treatments for patients.
Support and registry success
We encourage patients to enroll in our registry. It not only leads to discoveries, but it offers resources and support.
We still have a lot of work to do. Fortunately, we can now better understand the genetic events that trigger this rare disease and select treatment options because of those findings.